Temperature
Temperature monitoring
- Temperature monitoring is a vital but often neglected part of the management of a critically ill patient.
- Hypothermia causes coagulopathy and increases blood loss as well as depressing the functions of all organs. Rewarming increases cardiovascular instability because of vasodilatation and shivering. These patients often have substantial oxygen debt and this is exacerbated by shivering.
Temperature modalities
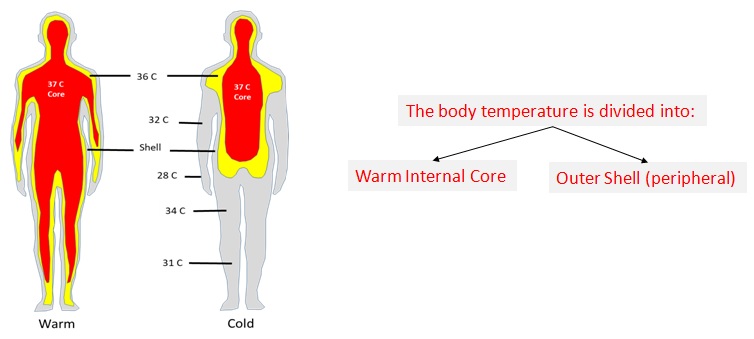
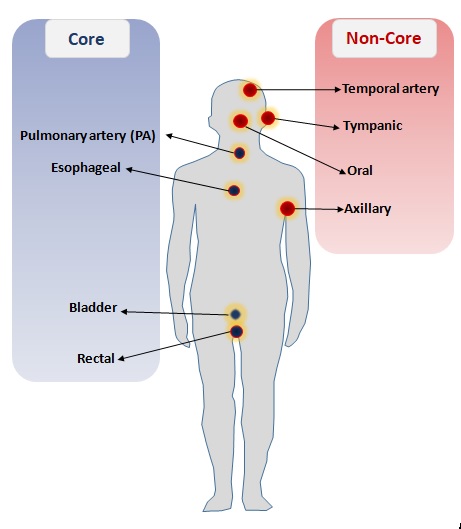
- Peripheral temperature reflects tissue perfusion and is affected by vasoconstriction and low cardiac output.
- Core Body Temperature: That temperature of the body which is least impacted by external factors or environment. Considered the true temperature of the body.
- Thermistors are used commonly for monitoring core temperatures and are based on the principle of changing resistance with temperature.
- Core temperature can be assessed rapidly using non‐invasive tympanic thermometers, but these are not always reliable in critically ill patients.
- For critical patient temperature monitoring, pulmonary artery temperature has long been the standard by which alternative core temperature modalities are measured against
- Esophageal and urinary bladder methods measure temperature continuously but have the disadvantage of being suitable only for intubated and sedated patients, or patients with a urinary catheter, respectively.
“The most accurate measure of temperature is core temperature taken typically via a bladder catheter or pulmonary artery catheter.” (Adler, etal. 2014)