Transcatheter Aortic Valve Implant/Replacement (TAVI/TAVR)
- A needle with syringe is inserted into the blood vessel.
- The syringe is removed (leaving the needle still in the vessel) and the guidewire is inserted into the vessel via the needle.
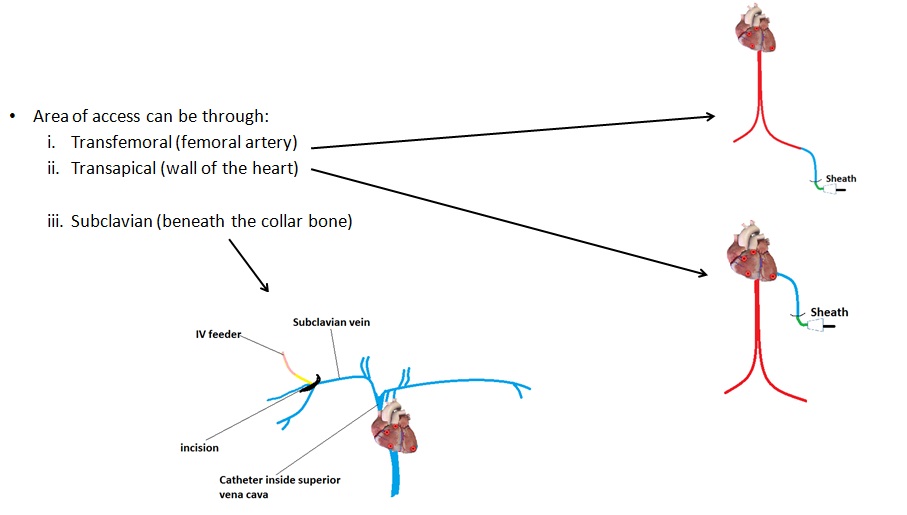
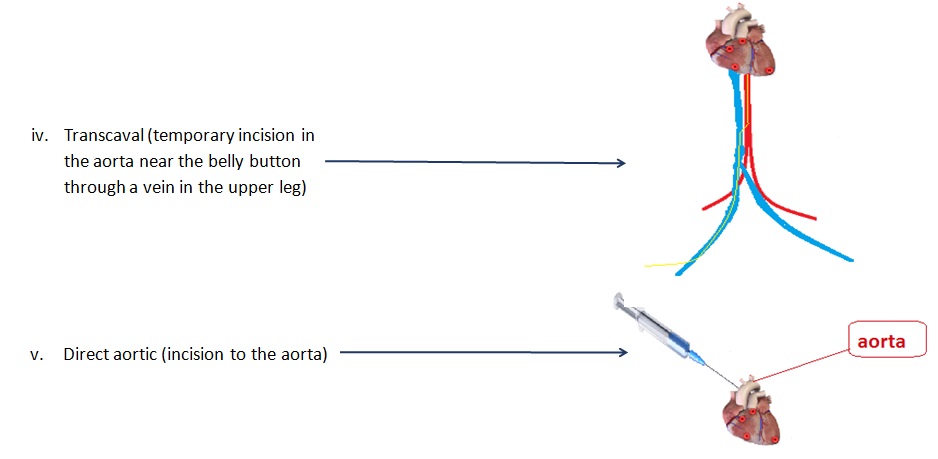
- Once the guidewire is in, the introducer sheath is inserted into the vessel along the guidewire.
- Once the introducer sheath is secure in place, the guidewire is removed and the guide catheter (J wire) is inserted through the introducer sheath.
- The guide catheter is navigated towards the heart, using real-time fluoroscopic images, then the aortic arch using C-arm x-ray machine that provides real-time fluoroscopic images.
- Radiopaque contrast media is injected through a port in the introducer sheath into the guide catheter to provide a view of the heart structure.
- The doctor will then decide upon the size of guidewire for the patient which will be used throughout the procedure.
- Heparin is injected into the vessel to prevent thrombosis or clotting.
- The guidewire is inserted into the vessel through the guide catheter, and then navigated to the coronaries where there is a blockage – this guidewire has a flexible tip to allow trackability.
- The guide catheter is then removed.
- The coronary guidewire is then twisted and turned (by its end outside the artery) to the site of the diseased heart valve – allows access to the site.
- The non-compliant balloon catheter is inserted along the guidewire to open up the valve.
- Then the NC balloon is removed and a balloon valvuloplasty catheter (contains the prosthetic valve stent) is inserted along the guidewire, navigated to the desired valve and inflated. The diameter of the balloon-stent can be adjusted and it will only be set in place once the balloon is pulled out of the valve-stent.
- Guidewire is removed along with the introducer sheath. The site of incision is sealed up